Formaldehyde had been produced and used commercially for over 100 years. Only recently, however,has it occupied a prominent place in the news. In 2006, the Federal Emergency Management Agency (FEMA) provided temporary housing(characterized as “toxic trailers” by the media) to hundreds of thousands of people who were rendered homeless by Hurricanes Katrina and Rita in August-September of 2005.
In 2010, US EPA (preceded by IARC in 2006 and followed by NTP in 2011) declared formaldehyde to be a known human carcinogen, based on its presumed ability to cause nasal and lymphohematopoietic cancers (especially acute myelogenous leukemia) in humans via the inhalation route. Concerned that EPA’s draft IRIS assessment for formaldehyde might not be entirely consistent with the established toxicological facts, a U.S. senator(Senator Vitter) persuaded EPA to submit its draft for review by the National Research Council of the National Academies.
That review, published in 2011,found “no clearly articulated framework for establishing causation on the basis of the weight and strength of evidence”, and confirmed that the proposed carcinogenic effects of formaldehyde in humans were inconsistent with the established facts of formaldehyde biology and toxicology, as currently understood, documented in the scientific literature, and previously summarized in government documents such as ATSDR’s Toxicological Profile for Formaldehyde. The important points made in the NAS review included the following:
(1) All of the known toxic effects of formaldehyde are confined to the portal of entry;
(2) Nasal cancer is induced in laboratory rats chronically exposed to levels of formaldehyde associated with sustained levels of cytotoxicity and compensatory cell proliferation (e.g., 10-15 ppm), but not at lower levels (i.e., <6 ppm, or at the NOAEL of 2 ppm). Such high levels of formaldehyde exposure are almost non-existent in humans, most of whom would find 6 ppm in air intolerable.
(3) Formaldehyde is formed endogenously in large quantities that are turned over rapidly; Blood levels of endogenous formaldehyde are generally in the range of 2-3 ppm, and its half-life in blood is only one and a half minutes.
(4) Even high levels of exogenous exposure related to occupation and diet are so small, compared to normal endogenous levels, that they have no detectable impact on blood levels.
To circumvent these daunting pharmacokinetic obstacles to the induction of cancer via a direct, mutagenic effect of inhaled HCHO on cells in bone marrow, a novel mechanism of leukemogenesis was proposed which required that (1) stem cells migrate from the bone marrow to nasal-associated lymphoid tissue, (2) form DNA adducts there with inhaled formaldehyde and (3) migrate back to the bone marrow and subsequently transform into leukemia cells. However, in a recent study published since the release of EPA’s draft IRIS assessment for formaldehyde, Lu et al. (2010)conclusively demonstrated that DNA adducts and cross-links formed by interaction with exogenous (i.e.,inhaled) formaldehyde were limited to the nasopharyngeal epithelium, while DNA adducts formed by interaction with endogenous formaldehyde were found in all tissues examined.
Specifically, DNA Adducts formed by inhaled formaldehyde could not be detected in either circulating white blood cells or bone marrow cells isolated from rats exposed to 10 ppm [13CD2]-formaldehyde for 1-5 days. These data indicate that the induction by inhaled formaldehyde of cancers at sites remote to the portal of entry is not biologically plausible.
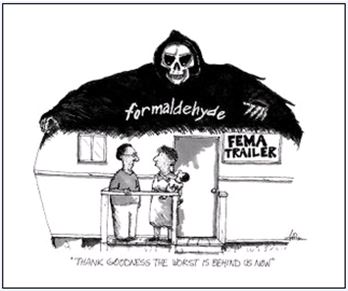
The Perception (since Katrina)
On August 29, 2005, Hurricane Katrina struck the Gulf Coast. 1 The Federal Emergency Management Agency (FEMA) purchased over 100,000 travel trailers&mobile homes to be used as temporary housing for over a quarter of a million homeless hurricane victims. 2 By 2006, some trailer residents were reporting headaches, coughs, nosebleeds, sick babies,&dying pets. 3,4 In December of 2007 and January of 2008, CDC began sampling the air in 519 trailers and mobile homes still occupied by Katrina victims, and detected an average of 77 ppb formaldehyde (HCHO) in air (range 0.3 – 590 ppb). 5 Newspapers characterized these results as “dangerously high levels of toxic gas” that exceeded ATSDR’s “limit for short-term exposure” [referring to ATSDR’s 40 ppb acute MRL] and were “nearly ten times the level for minimal risk” [referring to ATSDR’s 8 ppb chronic MRL]. 6 In May of 2007, More than 10,000 residents of these “toxic trailers” (as they were called by the media) were eventually enrolled in a class action lawsuit against a dozen different manufactures of the trailers. 6,7 In February of 2008, a local Mississippi Sierra Club chapter announced that 30 of 32 trailers tested by them registered “unsafe levels of formaldehyde”, and its conservation chair, Becky Gillette, told local newspapers that no one should live in untested FEMA trailers because “Too many people have gotten sick and died.” 6 The Sierra Club subsequently stated on its website that “Astonishingly, more people have been harmed by the formaldehyde in FEMA emergency housing than were harmed by Hurricane Katrina” (Almost 1400 deaths were confirmed in Louisiana alone from the direct effects of Katrina.)
In April of 2008, Congressional hearings were held to investigate allegations that CDC had ignored internal concerns that there was no recognized safe level of HCHO, that it could cause cancer and spontaneous abortions, and that HCHO in FEMA trailers portended “a pending public health catastrophe.” 8,9 The story spread, extending beyond the U.S. and FEMA trailers. Claiming that American studies had demonstrated the existence of a “serious cancer risk,” Australia’s biggest building union said formaldehyde is “as dangerous as asbestos”. 10 Parents all over America soon feared that their children were being poisoned by formaldehyde in school trailers (which, as it turns out, have the lowest HCHO concentrations of all trailers). 11,12
Subsequently, formaldehyde was officially declared a known human carcinogen by IARC 13, EPA 14 and NTP 15 in 2006, 2010 and 2011, respectively. (EPA’s decision was in draft form and is still pending, while that of IARC and NTP are final.) EPA concluded in its June 2, 2010 draft IRIS assessment for formaldehyde that there was sufficient evidence in humans of a causal relationship between inhaled fromaldehyde and nasopharyngeal cancer (NPC) and lymphohematopoietic (LHP) cancers, especially myeloid leukemia. 14 (In early 2011, the National Academies’ National Research Council reviewed this EPA draft document and recommended fundamental revisions. 16,17) In volume 88 of its Monographs, IARC had officially declared Formaldehyde a human carcinogen , based on nasopharyngel cancer, only, noting that “the mechanisms by which formaldehyde causes toxicity at distal sites are unknown, and “there is no experimental evidence to support… [the proposed] mechanisms.” 13 In October 2009, however, IARC updated their decision to include leukemia, thereby concurring more fully with EPA’s assessment. 18 Finally, NTP, which had listed formaldehyde as “reasonably anticipated to be a human carcinogen since 1981, changed that classification in its 12th Report on Carcinogens (2011 ROC) to “known to be a human carcinogen”, based on “sufficient evidence of carcinogenicity from studies in humans and supporting data on mechanisms of carcinogenesis.” 15
The Data
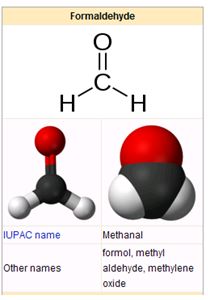
Formaldehyde has been produced commercially for
nearly 100 years, and is currently used by
many industries in a large array of products. It is a water-soluble (up
to 55%), irritating and highly reactive gas that has a distinct odor (threshold
0.5-1.0 ppm), and is ubiquitous in the environment. 19
More importantly,
from a toxicological perspective, formaldehyde is also a natural product of
metabolism. 19 According to ATSDR’s Toxicological Profile for
Formaldehyde, endogenous formaldehyde
is a normal metabolic product that is present at all times throughout the body
and is rapidly metabolized, and exogenous
formaldehyde induces adverse effects (predominantly eye, nose and throat
irritation in humans) only at the portal of entry, i.e., the upper respiratory
tract, in the case of inhalation exposures under 5-10 ppm 19
Distant
site effects occur only when the exposure dose (> 5-10 ppm) exceeds the local
capacity for absorption and metabolism 19. Even locally induced nasal tumors in
laboratory rats and mice require high (6-15 ppm) chronic exposures sufficient
to also cause sustained levels of cytotoxicity and cell proliferation; no
tumors at all are produced by sub-cytotoxic chronic doses of 2 ppm or less. 19, 20, 21, 22, 23 Exogenous doses sufficiently high to produce serious
local or (especially) systemic effects are rare in humans. (Most prominent
among those rare exceptions would be attempted suicides by formalin ingestion. 24)
Finally,
the rat data may very well overpredict the potential for nasal toxicity of
formaldehyde in humans by a considerable margin, because, compared to humans,
rats are obligate nose-breathers that exhibit much greater sensitivity to DNA
cross-link-formation in the nose. 25
As an essential metabolic intermediate in the
single-carbon pool, large amounts of endogenous formaldehyde (i.e., more than
50,000 milligrams) are produced, used, and/or detoxified by the human body
every day. 25 The very short half-life of formaldehyde in
the blood (1.5 minutes) maintains normal blood levels at a “mere” 2-3 ppm. 25 Nevertheless,
exogenous exposures are so much lower by comparison that even relatively high exposures
by either inhalation in the workplace (up to 15 ppm), or ingestion of foods
naturally high in formaldehyde (e.g., smoked meats, spinach, pears, and
provolone cheese), have no detectable impact on normal blood levels of endogenous
formaldehyde. 25
Formaldehyde is excreted in urine as formic
acid, and in exhaled breath as either CO2, or unchanged formaldehyde. Median concentrations of endogenous
formaldehyde in exhaled human breath are 4-10 ppb
26,27 and individual samples in one study ranged from 1.23 to
72.73 ppb 26. Thus, humans normally exhale formaldehyde
concentrations roughly a thousand times
higher than the 1-in-a-million risk level (0.01 ppb in air) that would correspond
to EPA’s recommended new Unit Risk for Formaldehyde (1 x 10-4 (ppb)-1 ). 14
EPA derived this new unit risk estimate by
(1) assuming that data from selected epidemiological studies demonstrated a
convincing, causal relationship between formaldehyde exposure and human cancer,
and (2) using zero-threshold-based models to extrapolate to lower doses. 14 However, the animal data clearly demonstrate
that cancer-induction by formaldehyde is a non-linear, high dose-dependent
phenomenon. The lowest cancer effect
level listed in ATSDR’s Toxicological Profile for Formaldehyde for
formaldehyde-induced nasal tumors in rats is 10,000 ppb, 6 hr/day, 5 days/wk,
for 24 months (i.e., most of a rat's lifetime).19
But, under identical conditions, 2,000 ppb had no effect. 19
In
support of their declarations that formaldehyde was a human carcinogen by the
inhalation route, IARC, USEPA, and NTP all cited the various studies of the National
Cancer Institute cohort as being the most convincing. 28,29,30,31 In
its review of EPA’s draft IRIS assessment for formaldehyde, the NAS/NRC
committee agreed with EPA’s choice of the NCI studies for the calculation of
unit risks, because “they are the only ones with sufficient exposure and
dose-response data for risk estimation,” but added that “the studies are not
without their weaknesses, and these need to be clearly articulated in the revised
IRIS assessment.” 16
The committee concluded that “the lack of
clear rationales for many conclusions weakened EPA’s arguments”, and
recommended substantial revisions, especially with regard to critically
evaluating individual studies, assessing the weight of evidence, and selecting
studies for derivation of RFCs and unit risk estimates. 16
Other authors have also questioned the biological plausibility of the
conclusion by IARC, USEPA, and NTP that inhalation exposures to formaldehyde
can cause cancer in humans at sites distant from the point of entry. 32,33,34,35,36
The most important of these is a recent study
by Lu et al (2010) in which male Fischer rats were exposed for 1 or 5 days to
10 ppm [13CD2]-formaldehyde, which enabled the
investigators to distinguish between DNA adducts and cross-links originating
from endogenous and inhalation-derived formaldehyde exposure. 35
High numbers of endogenous
formaldehyde-DNA adducts were present in all tissues examined, but exogenous [13CD2]-formaldehyde-DNA
adducts and cross-links formed only in rat nasal mucosa and not in any remote
tissues, including circulating white blood cells and bone marrow.
In addition, based on both in vivo and in vitro data, Lu et al. concluded that exogenous-DNA adducts were probably
too labile to last more than a day or two.
Together, these two observations strongly mitigate against a proposed mode of action whereby stem
cells would migrate from the bone marrow to nasal associated lymphatic tissue,
form DNA adducts with inhaled formaldehyde, then return to the bone marrow to eventually
become the initiated cellular precursors of leukemia.
According to
McKinney-Freeman and Goodell, circulating myeloid cells do not typically return
to bone marrow and proliferate, anyway.
36 Nevertheless, only Lu et
al. have provided clear evidence that “genotoxic effects at sites remote to the
portal of entry of inhaled formaldehyde are implausible.” 35 Previous labeling experiments could not
adequately distinguish between adducts formed with endogenous vs exogenous
formaldehyde, and simple scans of various tissues for radiation could not distinguish
actual adducts from metabolic incorporation of the label.
Nevertheless,
EPA, NTP and IARC have all concluded that relatively low levels of inhaled formaldehyde are known
to cause distal cancers in humans via unknown or proposed mechanisms for which
there is no supporting evidence. The principal
basis for those decisions is described, below.
Due to the sheer number of relevant (but weak and inconsistent) studies
in the literature, comments are made here only on the four NCI studies which
were deem by all four agencies to be of sufficient size and quality to support their
assumption of causality.
In
their study of 25,619 US workers employed at 10 plants between 1934 and 1994,
Hauptmann et al., (2003) found that
myeloid leukemia was significantly associated only with estimated peak formaldehyde exposures ≥4 ppm (95%
CI 1.27 to 9.43); there was also a marginally significant increase (95% CI 1.03
to 6.03) in workers with estimated average
exposures ≥ 1 ppm. 28 However, no
significant increase was observed with either cummulative exposure or duration
of exposure. The apparent association
between formaldehyde exposure in this cohort became even weaker with an
additional 10 years of follow-up. 29
Beane
Freeman et al., 2009 observed “little
evidence of association for any
lymphohematopoietic (LHP) malignancy [including myeloid leukemia] with average
intensity or cummulative exposure at the end of follow-up in 2004.” 29
In fact, the only
statistically significant increases observed by Beane Freeman et al. for any individual cancer type was for multiple
myeloma and Hodgkin’s Lymphoma (rather than for NPC and myeloid leukemia). And, the increases in multiple myeloma were reportedly
significant (SMR 2.04, 95% CI 1.01 to 4.12) only in the highest (estimated) peak
exposure category (≥ 4 ppm), and, oddly, in the controls, as well. 29 Hodgkin’s Lymphoma was significantly elevated
only in the intermediate (2 to 4 ppm) and highest (≥ 4 ppm) estimated peak exposure categories (95% CI 1.04 to
10.50 and 1.31 to 12.02, respectively) and in the intermediate (but not the highest) average intensity of exposure group (0.5 - < 1.0 ppm) with a 95%
CI of 1.41 to 9.31. 29
All
exposures were estimated, rather than measured, and effects were drawn from
death certificate data which, as the authors noted, “may lack specificity with
respect to sub-types of disease.” 29
With regard to nasopharyngeal cancer
in the NCI cohort, Hauptmann et al., 2004 concluded that their analysis was “consistent”
with an effect, but that “the number of deaths was too limited to enable a firm
conclusion.” 30 Finally,
in a case-control study of deceased funeral industry workers, Hauptmann et al.,
2009 estimated that, compared with
subjects who performed fewer than 500 lifetime enbalmings, the odds ratios of mortality
due to myeloid leukemia was significantly elevated (i.e., the confidence
interval did not include 1.0 ) only among those who performed embalmings for
more than 34 years (95% CI 1.2 to 12.5). 31
The author-identified limitations of this
study were the facts that (1) “exposure was estimated using interviews with
next of kin and coworkers”; (2) “there were relatively few deaths from myeloid
leukemia”, and (3) “there was a considerable amount of missing data that
required imputation for analysis.” 31
These were the principle human studies on which IARC, USEPA, and NTP based their decision to re-classify formaldehyde as a known human carcinogen.
Known Risk Factors for Nasopharyngeal Cancer in Humans
Nasopharyngeal cancer (NPC), though endemic in some
parts of the world (North Africa, Southeast Asia, China, and the far northern
hemisphere), occurs only rarely (< 1 person per 100,000 per year in the U.S.. 37, 38,41
The strongest risk factor for NPC in humans is Epstein-Barr Virus (EBV) infection, which has been known to be
associated with NPC since 1973. 39-46
EBV also causes acute infectious
mononucleosis and is closely associated with a number of other human diseases. 42,44
On the basis of its apparently causal association with Burkitt’s
lymphoma and nasopharyngeal tumors in humans, EBV has been classified by IARC
as a known human carcinogen. 41
Absent in normal
nasopharyngeal epithelial cells, EBV is detectable in all types of NPC (as well
as the associated preinvasive lesions), regardless of histological type or
degree of differentiation. 40,43,45
This differential presence of episomal EBV
genomes, and specific EBV gene products, strongly suggests that NPC cells are
clonal expansions of EBV-infected cells.
Initially, this association was most consistently demonstrated in the
most common form of NPC, i.e., non-keratinizing and undifferentiated NPC; however,
using Southern blot and in situ hybridization, the expression of EBV-encoded RNA
(EBER) has also been consistently detected in keratinizing squamous cell tumors
of the nasopharynx. 47,48,49
Other risk factors for NPC include genetic
susceptibility and diet (e.g., salt-cured fish and meat). 37,38,46
REFERENCES
The Perception:
1. CNN Special Report (August 29, 2005). http://www.cnn.com/SPECIALS/2005/katrina/.
2. The Seattle Times (March 12, 2010). “FEMA selling off Hurricane Katrina trailers tainted with formaldehyde.” by Spencer S. Hsu of the Washington Post. http://seattletimes.nwsource.com/html/nationworld/2011332997_trailers13.html
3. MSNBC (2006). Are FEMA trailers ‘toxic tin cans’? by Michael Brunker, Projects editor of MSNBC.com, July 25, 2006. http://www.msnbc.msn.com/id/14011193/from/ET/#storyContinued
4. Hattiesburg
American (2008). 'Erin
Brockovich of formaldehyde.' by Rick Jervis, Bay St. Louis, MS, May 2, 2008. http://dir.groups.yahoo.com/group/earthfirstalert/message/35115.
5. CDC (2008). Final Report on formaldehyde levels in
FEMA-supplied travel trailers, park models, and mobile homes. Centers for Disease Control, July 2,
2008. http://www.cdc.gov/nceh/ehhe/trailerstudy/pdfs/FEMAFinalReport.pdf
6. Arkansas Democrat-Gazette (2008). “FEMA homes ‘unsafe’ litigant warns.” By John Krupa, Little Rock, AR. Feb 14, 2008. http://www.toxic-trailer.com/pressreports/20080214b-press.html
(See alsdo: Sierra Club Insider (2008). “From toxic trailers to new standards.” http://action.sierraclub.org/site/MessageViewer?em_id=43383.0.)
7. Toxictrailers.org (2007). “Lawsuit on Formaldehyde Damages.”
http://www.toxictrailers.org/2007/05/info-on-class-action-lawsuit.html.
8. Committee on Science & Technology (2008). “Toxic trailers – Toxic lethargy: How the Centers for Disease Control and Prevention has failed to protect the public health.” Majoprity Staff Report. Subcommittee on Investigations and Oversight. Committee on Science & Technology. U.S. House of Representatives. September 2008.
http://www.toxic-trailer.com/govinvdocs/ATSDR_Staff_Report_9.22.08.pdf
9. Associated Press (2008). “Scientist: CDC bosses ignored trailer warnings.” Washington, DC.
10. ABC News (April 24, 2008). “Formaldehyde is the next asbestos: CFMEU”
http://www.abc.net.au/news/2008-04-24/formaldehyde-is-the-next-asbestos-cfmeu/2414554.
11. Daily Herald (Chicago) (2008). “Are school trailers safe? You won't know in Illinois.” By Kerry Lester. http://67.151.102.2/story/?id=164635
12. The Courier News (2008). “Officials: Air OK in mobile classrooms.” By David Gialanella of the Courier News (Elgin IL), April 24, 2008. http://www.highbeam.com/doc/1N1-1209D3ED2AD0DC78.html
13. IARC (2006). Formaldehyde, 2-Butoxyethanol and 1-tert-Butoxypropan-2-ol. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Volume 88. Lyon, France: WHO, 2006. (Formaldehyde section is on pp 39-325).
14. EPA (2010). Toxicological review of formaldehyde (DRAFT) – Inhalation assessment. In support of summary information on the integrated risk information system (IRIS). Vol III of IV, Quantitative Assessment, Chapter 6: Major Conclusions in the Characterization of Hazard and Dose Response. U.S. Environmental Protection Agency, Washington, DC, June 2, 2010.
15. NTP (2011). Formaldehyde. pp 195-205 In: 12th Report on Carcinogens. National Toxicology Program, Public Health Service, U.S. Department of Health and Human Services.
16. NAS/NRC (2011). Review of the Environmental Protection Agency’s draft IRIS assessment of formaldehyde. National Research Coincil of the National Academies. Division of Earth and Life Studies. The National Academies Press, Washington, DC, 2011.
17. New York Times (2011). “NAS reviewers slam EPA’s formaldehyde assessment.” By Jeremy P. Jacobs, April 8, 2011.
18. Metzger Law Group (2011). “IARC declares formaldehyde a human carcinogen.”
The Data:
19. ATSDR (1999). Toxicological Profile for Formaldehyde. Agency for Toxic Substances and Disease Registry. Public Health Service. U.S. Department of Health and Human Services, Atlanta, GA.
20. Swenberg JA, Kerns WD, Mitchell RI, et al (1980). Induction of squamous cell carcinomas of the rat nasal cavity inhalation exposure to formaldehyde vapor. Cancer Res 40: 3398-3402.
21. Kerns WD, Pavkov KL, Donofrio DJ, et al. (1983). Carcinogenicity of formaldehyde in rats and mice after long-term inhalation exposure. Cancer Res 43: 4382-91.
22. Monticello TM, Swenberg JA, Gross EA, et al. (1996). Correlation of regional and nonlinear formaldehyde-induced nasal cancer with proliferating populations of cells. Cancer Res 56: 1012-22.
23. Kamata et al. (1997). Results of a 28-month chronic inhalation toxicity study of formaldehyde in male Fisher-344 rats. J Toxicol Sci 22: 239-54.
24. Pandey CK, Agarwal A, Baronia A, and Singh N (2000). Toxicity of ingested formalin and its management. Hum Exper Toxicol 19: 360-66.
25. Sullivan, John B. andKrieger Gary R. (2001). Formaldehyde. Chapter 95 In: Clinical Environmental Health and Toxic Exposures. Pp. 1006-1013.
26. Moser, B; Bodrogi, F; Eibl, G; Lechner, M; Rieder, J; and Lirk, P (2005). Mass spectrometric profile of exhaled breath – field study by PTR-MS. Respir Physiol Neurobiol 145: 295-300.
27. Kushch, I; Schwartz, K; Schwnetner, L; Baumann, B; Dzien, A; Schmid, A; Unterkofler, K; Gastl, G; Španĕl, P; Smith, D; and Amann, A (2008). Compounds enhanced in a mass spectrometric profile of smokers” exhaled breath versus non-smokers as determined in a pilot study using PTR-MS. J Breath Res 2 026002. http://iopscience.iop.org/1752-7163/2/2/026002.
28. Hauptmann et al. (2003). Mortality from lymphohematopoietic malignancies among workers in formaldehyde industries. JNCI 95(21): 1615-23.
29. Beane Freeman et al. (2009). Mortality from lymphohematopoietic malignancies among workers in formaldehyde industries: the National Cancer Institute cohort. JNCI 101(10): 751-61.
30. Hauptmann et al. (2004). Mortality from solid cancers among workers in formaldehyde industries. Am J Epidemiol 159: 1117-30.
31. Hauptmann et al. (2009). Mortality from lymphohematopoietic malignancies and brain cancer among embalmers exposed to formaldehyde. J Natl Cancer Inst 101(24): 1696-1708.
32. Collins JJ, Ness R, Tyl RW, Krivanek N, Esmen NA, Hall TA (2001). "A review of adverse pregnancy outcomes and formaldehyde exposure in human and animal studies," Regul Toxicol Pharmacol. 2001 Aug;34(1):17-34.
33. Heck, Henry d’A. and Casanova, Mercedes (2004). The implausibility of leukemia induction by formaldehyde: a critical review of the biological evidence on distant-site toxicity. Regul. Toxicol. Pharmacol. 40: 92-106.
34. Pyatt, D; Natelson, E; and Golden, R (2008). Is inhalation exposure to formaldehyde a biologically plausible cause of lymphohematopoietic malignancies? Regulat Toxicol Pharmacol 51: 119-33.
35. Lu, Kun; Collins, Leonard B.; Ru, Hongyu; Bermudez, Edilberto, and Swenberg, James A. (2010). Distribution of DNA adducts caused by inhaled formaldehyde is consistent with induction of nasal carcinoma but not leukemia. Toxicol. Sci. 116(2): 441-451.
36. McKinney-Freeman S and Goodell MA (2004). Circulating hematopoietic stem cells do not efficiently home to bone marrow during homeostasis. Exp Hematol 32: 868-76.
Known Risk Factors:
37 Casciato DA and Territo MC (2009). Manual of Clinical Oncology, Sixth Edition. (Dennis A. Casciato and Mary C. Territo, Eds.) Wolters Kluwer/Lippincott Williams & Wilkins, New York, NY, page 155.
38. Abraham, Gulley and Allegra (2010). The Bethesda Handbook of Clinical Oncology, Third Edition. (Lane Abraham, James L. Gulley and Carmen J. Allegra, Eds.) Wolters Kluwer/Lippincott Williams & Wilkins, New York, NY, page 22.
39. Kieff, Elliot (1995). “Epstein-Barr Virus – Increasing evidence of a link to carcinoma.” NEJM 333 (11): 724-26.
40. Pathmanathan et al., (1995). Clonal proliferations of cells infected eith Epstein-Barr virus in pre-invasive lesions related to nasopharyngeal carcinoma. NEJM 333 (11): 693-726.
41. IARC (1997). Epstein-Barr virus and Kaposi’s sarcoma herpes virus/human herpes virus 8. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Volume 70. Lyon, France: WHO, 1997.
42. Pagano, JS (1999). Epstein-Barr virus: the first human tumor virus and its role in cancer.
43. Niedobitek, G (2000). Epstein-Barr virus infection in the pathogenesis of nasopharyngeal carcinoma. J Clin Pathol : Mol Pathol. 53: 248-54.
44. Kawa, K (2000). Epstein-Barr virus – associated diseases in humans. Int J Hematol. 71(2): 108-17.
45. Jin-Ching Lin et al., (2010). Detection of Epstein-Barr virus DNA in the peripheral-blood cells of patients with nasopharyngeal carcinoma: relationship to distant metastasis and survival. J Clin Oncol 19L1): 2607-15.
46. Mayo Clinic Online (2011). Nasopharyngeal Carcinoma: Risk Factors. http://www.mayoclinic.com/health/nasopharyngeal-carcinoma/DS00756/DSECTION=risk-factors.
47. Raab-Traub N, Flynn k, Pearson G, et al. (1987). The differentiated form of nasopharyngeal carcinoma contains Epstein-Barr virus DNA. Int J Cancer 39: 25-29.
48. Pathmanathan R, Prasad U, Chandrika G et al. (1995). Undifferentiated, non-keratinizing, and squamous cell carcinoma of the nasopharynx: Variants of Epstein-Barr virus-infected neoplasia. Am J Pathol 146: 1355-67.
49. Nicholls JM, Agathanggelou A, Fung K, et al. (1997). The association of squamous cell carcinomas of the nasopharynx with Epstein-Barr virus shows geographic variation reminiscent of Burkitt’s lymphoma. J Pathol 183: 164-8.




Comments