The subject of endocrine disruption is not particularly new, with extensive scientific and regulatory attention to endocrine disrupting chemicals (EDCs) over the last 20 years or so. A common definition, from the World Health Organization/International Programme on Chemical Safety, is:
An endocrine disruptor is an exogenous substance [i.e. a substance not originating in an organism] or mixture that alters function(s) of the endocrine system and consequently causes adverse health effects in an intact organism, or its progeny, or(sub)populations.”
Quite a few natural and synthetic chemicals exhibit endocrine activity but, in spite of 20 years of research, the field of endocrine disruption continues to be ill-defined and highly controversial. Two of the current controversies revolve around the related concepts of low-dose effects and non-monotonic dose response curves (NMDRC).
In the field of toxicology, a bedrock principle is that “the dose makes the poison,” meaning that a toxicological response is generally expected to increase (or decrease) monotonically with increasing dose. In contrast, the NMDRC concept suggests that the slope of the dose-response curve for endocrine active compounds may change from positive to negative, or vice versa, with increasing dose, for example resulting in U-shaped or inverted U-shaped dose-response curves.
Although NMDRCs will not be further discussed in this article, interested readers can learn more in a recent draft report on the topic from the US Environmental Protection Agency, which highlights the lack of reproducible evidence regarding NMRDCs and illustrates some of the key shortcomings of the research purportedly showing NMDRCs.
One of the challenges in discussing low-dose effects is the lack of a clear definition. Low-dose effects are generally considered to mean effects that occur at levels below the no-effect levels established in traditional toxicology studies. More pertinently for this article, the term is sometimes more specifically defined as effects that occur in the range of typical human exposures.
Accordingly,for studies focused on evaluating potential low dose effects and NMDRCs, dose selection is a critical and controversial study design parameter. In this regard, a recent study claiming that the common chemical bisphenol A (BPA), considered by some to be an endocrine disruptor, caused adverse effects at a human-relevant dose was of particular interest. The authors signaled the significance of the low dose by referring to its human relevance at least six times in the body of the relatively short paper. If it’s worth repeating six times, it must be important, right?
Important or not, the new study,funded by a grant from the National Institute of Environmental Health Sciences (NIEHS), is not unique in touting the human relevance of the dose tested. Inspection of a list of NIEHS-funded studies addressing BPA reveals another 24 that also highlight the human relevance of the dose(s) tested, although none so obsessively as the most recent example.
At first blush, we should congratulate NIEHS for consistently funding studies of such direct relevance to human health. But before congratulations are offered, maybe we should take a closer look.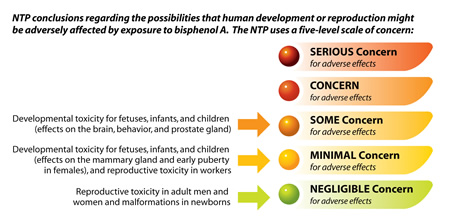
Does the science match the warning level? Credit: National Institute of Environmental Health Sciences.
In the new study, mice were provided a diet that contained 5 mg BPA/kg of diet (5parts per million). Based on food consumed, the authors estimated BPA intake to be 20 µg/mouse per day. Although the authors didn’t report the bodyweight of their mice, we can estimate, based on standard weights for the mouse strain tested, that the daily intake was on the order of 1,000 µg BPA/kg bodyweight per day.
For this dose to be human-relevant as claimed, people should be consuming approximately the same amount of BPA on a bodyweight adjusted basis, and therein lies the rub. Although characterized as a human-relevant dose, extensive data have shown that typical human exposures to BPA are orders of magnitude lower.
It is well established that BPA has a half-life in the body of only a few hours and is quantitatively excreted in urine in the form of a biologically inactive metabolite. As stated by the European Food Safety Authority in its comprehensive BPA exposure assessment, “[u]rine is therefore the matrix of choice for biomonitoring, and the urinary concentration of total (unconjugated plus conjugated) BPA is the biomarker of choice to estimate BPA exposure.”
Recognizing this, numerous biomonitoring studies that measure total BPA in urine have been conducted around the world, most notably population-scale studies conducted by the US Centers for Disease Control (CDC) and Health Canada. These studies consistently show that human exposure to BPA is typically less than 0.1 µg BPA/kg bodyweight per day, which is approximately 10,000-fold lower than the so-called human-relevant dose given to mice in the recent study.
The same large discrepancy between typical human exposure and the dose(s) tested ispresent in all of the other NIEHS-funded studies that claim human-relevant doses were used. Surprisingly, neither the recent study, in spite of the repeated references to a human-relevant dose, nor any of the other NIEHS-funded studies, make any mention whatsoever of these well-established,scientifically robust and widely accepted human exposure measurements.
Insteadof relying on these population-scale studies to provide a scientifically solid baseline of actual human exposures, all of the NIEHS-funded studies tested doses (or in vitro concentrations) comparable only to levels reported to be present in human blood in various small-scale studies. But by doing this, the NIEHS-funded studies also ignore the consensus of biomonitoring and bioanalytical experts that measurement of BPA in human blood is not a reliable method for estimating exposures, most prominently including CDC and the US Food and Drug Administration.
Experts from these authorities have made no secret of their critical views of the validity of BPA blood measurements:
“Taken together, these results suggest that blood or its products (serum/plasma) is an unfavorable matrix for the biomonitoring of BPA exposure in the general population.” (CDC, Ye et al. 2012)
“However, for the reasons that follow, it is seldom possible to verify that serum concentrations of these compounds are valid measures of exposure.”(CDC, Calafat et al. 2013)
“The lack of concordance with intake estimates … based on fullyvalidated urinary measurements of BPA conjugates … makes it likely thatmeasurements of ng/ml levels of aglycone BPA in human plasma were compromised by the ubiquitous BPA contamination in the environment.” Doerge et al. 2010
“The simplest explanation for this discordance is sample contamination leading to false positive determinations of aglycone BPA in human blood, which otherwise would contain levels undetectable by any current analytical methodology.”(FDA, Twaddle et al. 2010)
“[B]lood biomarkers of BPA likely represent only contamination.” (Wolff 2011
So what’s going on here? All of the 25 NIEHS-funded studies make similar claims of human-relevant doses, all rely on data considered by the world’s experts to be questionable at best, and all ignore the most reliable measures of human exposure. The result is that the studies are of very limited relevance to human health since the reported effects occur at doses far above typical human exposures, not at human-relevant doses as claimed.
Can all of this be the result of coincidence? No, NIEHS has stated that studies it supports will focus on “low environmentally relevant doses of BPA.” We can only conclude that being off by a factor of 10,000 is close enough for NIEHS-supported research. But rather than congratulating NIEHS, two important questions remain: How did NIEHS and its grantees get it so wrong – 25 times and counting – and how many millions of dollars of precious grant money has been spent on research that can be of only very limited relevance to address important public health issues related to BPA?
Note in proof: After writing this article, another NIEHS-funded study was published with the same claim of human-relevant doses. It’s now 26 times and counting.





Comments