According to the albino hairless mouse model, both UVB and UVA can be involved in the development of cutaneous cancers including squamous cell carcinomas (SCC) and basal cell carcinomas (BCC). However, the relative efficiency of UVA in inducing these carcinomas is approximately 10,000 times lower than UVB and much higher doses of UVA are required [2].
Both UVA and UVB act by causing programmed cell death [apoptosis] which has been linked to carcinogenesis [3]. Thus, ideally, sunscreen products should provide efficient protection against UVB and UVA radiation. The natural human sunburn cycle (without the use of any sun lotions or sunscreens) is approximately one week in length (7 days) from start to finish. Macroscopically, it consists of three phases including inflammation, new tissue formation, and apoptosis (visible peeling).
The inflammatory phase consists of redness and inflammation commencing 20-30 minutes from the time of initial sun exposure. It spans grossly 2-3 days, but can last up to 5 or 6 days depending upon UV intensity. New tissue formation is stimulated some time after initial exposure and it is complete within one week. In the last apoptotic phase, the top layer of dead skin cells sloughs off to reveal a new tissue layer beneath. This process follows on from the inflammatory phase and is complete approximately 7 days following exposure. While there is some redness and inflammation following initial exposure and on day 1, the inflammatory reaction seems to peak on day 2.
The onset of apoptosis (visible peeling) occurs between day 2 and day 3 while there is an accompanying decrease in redness and inflammation. The peak of apoptosis, visible as peeling, is seen on day 4 which declines gradually on day 5 and 6 as the dead cells fall away from the skin. By day 7, recovery is usually complete and the old cells have been replaced by new ones. Previously, it has been shown that sunburn can also occur despite the use of sunscreen (15 SPF) during winter months in a temperate climate. In addition, sunburn may still occur while wearing stronger sunscreens (30 SPF). Although they may attenuate or even eliminate the first phase of redness and inflammation, the second and third phases may not be prevented.
Since it is the last apoptotic phase that has been linked to carcinogenesis, this would appear to reflect an inherent weakness in the general composition of many sunscreens available to the consumer. It also brings into question the efficacy and safety of sunscreens which effectively block inflammation, but are unable to prevent peeling following sun exposure in providing protection against skin cancer [4]. Thus, in the current case-study two new sunscreen formulations were tested for their respective ability to block peeling, or, apoptosis following exposure to solar radiation.
The first was a preparation of pure zinc oxide [7.5%] in a creme base rather than the microfine or nano form which is currently a popular ingredient of sunscreens [5]. The second was a preparation of melanin [50 mg/ml] extracted from black sesame in a creme base containing zinc oxide [7.5%]. Zinc oxide was chosen for its property as the broadest spectrum UVA and UVB reflector that is approved for use as a sunscreen by the FDA [6]. Moreover, it is photostable [7]. Zinc oxide has the added advantage of sitting on the surface of the skin without being absorbed into it which may not be the case with the microfine or nano form.

Melanin was chosen because it is the natural sunscreen of the human body, which usually protects itself from solar radiation by increasing melanin production. It ranges in colour from red and yellow {pheomelanin} to brown and black {eumelanin} with the latter being the most effective [8]. However, certain individuals are not able to produce enough melanin and this can result in sunburn. Thus, there is reason to suppose that it may be the most suitable ingredient for a commercial sunscreen. Previously, it has been shown that bacterial-derived melanin can provide photoprotection against UVA-induced cell death [9].
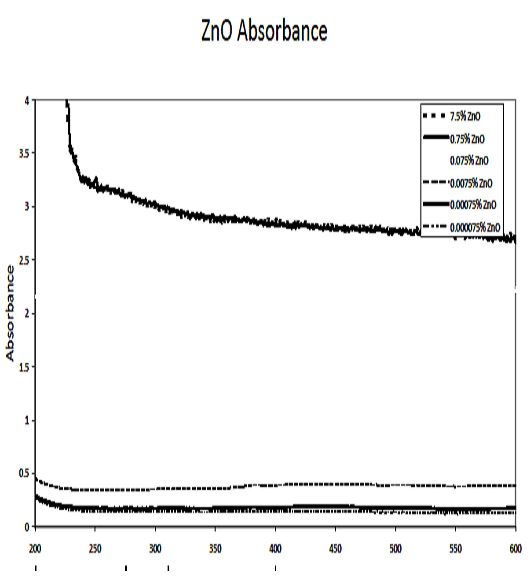
Therefore, in this study, melanin derived from black sesame [Sesamum indicum] was selected for its potential application as an active sunscreen {courtesy of Lingonberry Organic Foodstuffs, China}.Absorbance studies carried out on the zinc oxide and melanin confirmed these claims {courtesy of Matthew Brichacek and Professor PJ Hergenrother’s Lab}. The zinc oxide at 7.5% was found to be a good reflector in the UVB and UVA ranges. The melanin at .4 mg/ml was found to be a good reflector in the UVB and UVA2 (320-340 nm) ranges, while it was only moderate in the UVAI range (340-400 nm).
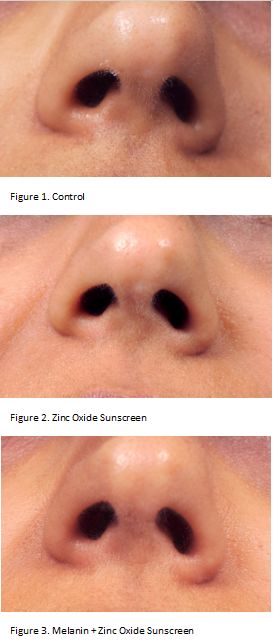
Since zinc oxide appeared to be an adequate sunscreen at this concentration, it seemed reasonable that these two sunscreen ingredients should form an even more effective sunblock together. The experimental model was similar to the one previously described [4]. The subject sat outdoors or walked at noon facing the direct sunlight on a clear, sunny day. Each experiment lasted between 30 and 60 minutes following the application of sunscreen, which was applied at least 15 minutes prior to exposure. The control experiment was performed under the same conditions without the application of any sunscreen or sun lotion. Photographs of the face were taken 48 to 72 hours from the time of commencement of initial sun exposure which was deemed as 0 hours at approximately noon on the day of trial. All experiments were conducted between the months of late May, June, August, and early October at Ambleside beach or on the mountainside in West Vancouver, British Columbia (Canada).
These same results were repeatedly observed under comparable conditions. A slight pinkish sunglass line appeared on the nose following the trial with the zinc oxide sunscreen. Although probably representing some degree of immediate pigment darkening [IPD] and persistent pigment darkening [PPD] in response to UVA radiation, the line was none of the expected melanin colours in the eumelanin or pheomelanin range {brown, black, yellow, or red}. In support of this, as UV intensity increases in summer months, the subject experiences an inefficient pigment darkening process {IPD within an hour} simultaneously with sunburn including all three phases of inflammation, new tissue formation, and apoptosis. In addition, the dark flesh-pink coloration only occurred on the nose and slightly on the cheeks while there was no sunglass line on the cheeks with the zinc oxide sunscreen.
This seems to follow a localized sunburn pattern in susceptible areas like the nose and cheeks rather than the usual diffuse suntan pattern suggesting another component to the reaction. In contrast, it is interesting to note that the suntan pattern is ordinarily uniform because pigment-producing melanocytes are evenly distributed throughout the basal epidermal layer of the human skin. Moreover, IPD is said to fade rapidly in 24 hours and PPD within several days, while this coloration persisted for up to a week. Therefore, there could be some overlap with the inflammatory phase of the sunburn cycle suggesting a combination of IPD, PPD, and redness caused by inflammation. There was also a slight stinging and burning sensation on the face up to 24 hours following sun exposure consistent with an inflammatory reaction. In the case of the melanin sunscreen, a sunglass line was visible after one hour of sun exposure on both nose and cheeks while no acute redness or inflammation was observed. Once again, the sunglass line was pinkish and there was some slight stinging during sun exposure possibly indicating a little sunburn. However, the coloration on the nose and cheeks was more uniform with this sunscreen suggesting a greater ratio of IPD/PPD to inflammation than with the first sunscreen. In addition, the colour faded within several days.
This could potentially be an interesting observation because while UVA can also cause erythema, which is unlikely to serve any supportive function, IPD, or, delayed UVA tanning may actually play a protective role against UVB exposure [10]. Since there was no peeling even 96 hours after sun exposure with either sunscreen, this indicates that both these formulations may be somewhat effective in preventing the apoptotic phase, but not necessarily the inflammatory phase, of UVB-induced sunburn by uncoupling the two events [Figures 1, 2&3].
The inflammation may also represent some degree of UVA-induced erythema. As zinc oxide is a known UVAI blocker at 7.5% and since it is UVAI that causes IPD, it is unlikely to be the sole cause of the change in coloration observed in these trials.
Although not an ideal result, these two sunscreen formulations are preferable to those which prevent the inflammatory but not the apoptotic phase of sunburn which has been linked to carcinogenesis. In fact, erythema and IPD have been chosen as the current end points for evaluating the sun protection factor {SPF} of sunscreens, but some authors have suggested using other end points which are more representative of long term UV cutaneous damage such as global DNA damage or sunburn cells/apoptosis for this reason.
References
1. Bernerd F, ViouxC, Lejeune F, Asselineau D. European Journal of Dermatology 13(3): 242-249, 2003
2. Routaboul C, Denis A, Bohbot M. European Journal of Dermatology 12(5): 439-444, 2002
3. Siddoo-Atwal C. Indian Journal of Ecology 36(2):103-110, 2009
4. Siddoo-Atwal, C. Sunburn with Sunscreen – A Case-Study.Science 2.0; published on-line April20, 2011
5. Pinnell SR,Fairhurst D, Gillies R, Mitchnick MA, Kollias N. Dermatologic Surgery 26(4): 309-314, 2000
6. US Food and DrugAdministration. http://www.fda.gov/RadiationEmittingProducts/RadiationEmittingProductsan...
7. Mitchnick MA,Fairhurst D, Pinnell SR. Journal of the American Academy of Dermatology 40(1): 85-90, 1999
8. Chintala S, LiW, Lamoreux ML, Ito S, Wakamatsu K, Sviderskaya EV, Bennett DC, Park Y-M, GahlWA, Huizing M, Spritz RA, Ben S, Novak EK, Tan J, Swank RT. Proceedings of the National Academy of Sciences of the United States of America 102(31): 10964-10969, 2005
9. Geng J, Tang W,Wan X, Zhou Q, Wang X-J, Shen P, Lei T-C, Chen X-D. Journal of the European Academy of Dermatology and Venereology 22(7): 852-858, 2008
10. Kaidbey KH,Kligman AM. Archives of Dermatology 114:46-48, 1978




Comments