Lung cancer is one of the top killers of people. Once patients receive a diagnosis, chemotherapy is common but accurate predictions about whether or not this treatment will help are impossible.
New treatments are always in the works but the road from article on Science 2.0 to FDA approval is long. Before anything can incur the costs of a clinical trial, it has to show success in animal models.
"Animal models may be the best we have at the moment, but all the same, 75 percent of the drugs deemed beneficial when tested on animals fail when used to treat humans," explains Prof. Dr. Heike Walles of the Fraunhofer Institute, who is working on a 3-D test system that can help.
Essentially what they have done is to recreate the human lung in miniature – with a volume of half a cubic centimeter, each model is no bigger than a sugar cube.
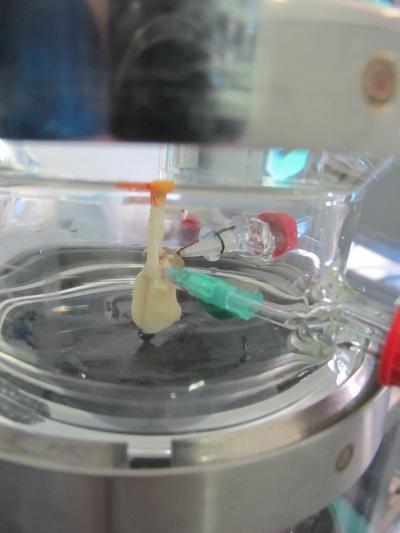
3-D Lung tumor model helps researchers to test medications.
Credit: © Fraunhofer IGB
The biological model is based human lung cancer cells growing on tissue. An artificial lung is created, a bioreactor is used to make it breathe and to pump a nutrient medium through its blood vessels in the same way our bodies supply our lungs with blood. The reactor also makes it possible to regulate factors such as how fast and deeply the model lung breathes.
In a parallel effort, scientists at the Department of Bioinformatics at the University of Würzburg are working up computer simulation models for different patient groups. These are necessary because patients may have genetic variations that inhibit therapies from having the desired effect. Comparing the theoretical and biological models allows each research group to optimize their results.
Having constructed the lung tissue, Walles reports that "treatments that generate resistance in clinics do the same in our model." Researchers are now planning to explore the extent to which their artificial lung can be used to test new therapeutic agents. Should resistance crop up during testing, doctors can opt to treat the patient with a combination therapy from the outset and thus side-step the problem. Thinking long-term, there is even the possibility of creating an individual model lung for each patient. This would make it possible to accurately predict which of the various treatment options will work. The required lung cells are collected as part of the biopsy performed to allow doctors to analyze the patient's tumor.
On the trail of metastases
The model lung can also help researchers to better understand the formation of metastases; it is these that often make a cancer fatal. "As metastases can't be examined in animals – or in 2-D models where cells grow only on a flat surface – we've only ever had a rough understanding of how they form.
3-D lung tissue makes it possible to perform metastases analysis. In order to travel through the body, tumor cells alter their surface markers – in other words, the molecules that bind them to a particular area of the body. Cancer cells are then free to spread throughout the body via the body's circulatory system before taking up residence somewhere else by expressing their original surface markers.
The scientists plan to use their model lung's artificial circulatory system to research exactly how this transformation occurs. And in doing so, they may someday succeed in developing medication that will stop metastases from forming in the first place.




Comments