Currently approved flu vaccines are less effective in the elderly, yet an estimated 90% of influenza-related deaths occur in people over 65. A paper published on January 23rd in PLOS Pathogens reports on the challenges scientists encountered when they were trying to develop a better flu vaccine.
Because immune systems in older people are generally less responsive to vaccination, Jay Evans and colleagues from GlaxoSmithKline Vaccines in Hamilton, USA, were testing so-called adjuvants—vaccine components that provoke a stronger immune reaction—that could be added to the regular flu vaccine cocktail to prompt even weaker immune systems to develop protective immunity against subsequent encounters with the flu virus.
A second possible way to increase vaccine efficiency against respiratory viruses is by nasal delivery. This stimulates both local and systemic (body-wide) immunity. And because the respiratory mucosa is the first line of defense against influenza, enhancing immunity locally in this tissue is likely beneficial.
To explore both ways to boost immunity together, the scientists vaccinated mice intra-nasally with a typical flu vaccine cocktail combined with an adjuvant called CRX-601, and then exposed them to flu virus that was related but not identical to the strains used in the vaccine.
On the positive side, they found that all vaccinated mice survived the lethal influenza virus challenge and showed flu-specific protective antibodies both locally and systemically. However, they also found that after the mice were challenged, they initially got quite sick and lost weight, before starting to recover after about a week.
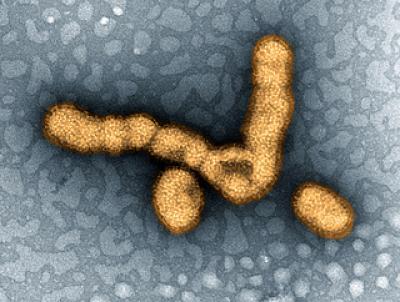
This image shows H1N1 influenza virus particles.
(Photo Credit: NIAID, Flickr)
When they examined the reason for this illness, they found that the vaccination had caused expansion of a group of flu-specific immune cells that secrete a molecule called Th17 into the blood. They also saw that the Th17 did not contribute to fighting the virus but instead caused an unhealthy immune reaction that made the mice sick.
To test whether this was caused by the adjuvant, by the nasal delivery, or both, they used the same vaccine-adjuvant combination but delivered it subcutaneously (similar to a regular flu shot). These mice did not get transiently sick after virus challenge and, like the ones vaccinated in the nose, all survived. Similarly, intra-nasal vaccination without the adjuvant did not elicit the unwanted Th17 response. However, most of these mice died following influenza virus challenge, demonstrating that the adjuvant makes the vaccine more protective. These experiments show that the Th17-mediated adverse effects are caused by a combination of the CRX-601 adjuvant and the intra-nasal delivery.
The mice in all the experiments up to this point had been "naïve", that is, they had never encountered and survived flu viruses. However, the majority of adult humans have some degree of pre-existing immunity to influenza (from flu shots or from having been ill with the flu before). When the scientists tested the response to intra-nasal vaccination with the flu cocktail plus CRX-601 adjuvant in mice that had survived a flu-infection before, they found that these mice did not show the detrimental Th17 responses and the associated illnesses after viral challenge.
So while it is clear that animal testing of flu vaccines is a complicated business, in the end, the scientists conclude that "intranasal immunization for influenza with a vaccine that contains an adjuvant like ours need not be ruled out for the elderly, as they are likely to have pre-existing immunity that prevents the TH17 adverse effects." More generally", they say "our study draws attention to a need for a more thorough characterization of immune responses following intra-nasal vaccinations, particularly when novel adjuvants are present in the vaccine formulations."




Comments