Almost 90 percent of children and adults with a highly aggressive form of acute lymphoblastic leukemia (ALL) showed no evidence of cancer after receiving a personalized cell therapy that reprograms a patient's immune system.
In pilot studies of bio-engineered T cells that attack leukemia, 24 of 27 patients (89%) experienced complete responses within 28 days after treatment. In all, 27 patients received the treatment - 22 children treated at The Children's Hospital of Philadelphia and five adults treated at the Hospital of the University of Pennsylvania.
Pediatric oncologist Stephan A. Grupp, M.D., Ph.D., of The Children's Hospital of Philadelphia and a Professor of Pediatrics at the Perelman School of Medicine of the University of Pennsylvania, presented outcomes and follow-up results of this immunotherapy clinical trial for pediatric and adult patients with ALL in a press program today at the annual meeting of the American Society of Hematology (ASH) in New Orleans.
"Our results serve as another important milestone in demonstrating the potential of this cell therapy for patients who have no other therapeutic options," said study author Grupp. "We are also very excited that this approach has worked and been safe in patients who have relapsed after a bone marrow transplant."
All the patients had high-risk ALL that recurred after initial treatment or resisted that treatment from the start. Patients received bioengineered "hunter" T cells called CTL019 cells.
The first child to undergo this therapy, 8-year-old Emily Whitehead, remains cancer-free since her T cell treatment in April 2012, and has gone on to enjoy typical childhood activities like going to school and playing with her dog, Lucy. Emily has appeared prominently in news articles since her doctors announced dramatic findings during the December 2012 ASH meeting.
In follow-up assessments, the researchers reported six relapses among the 24 patients with complete responses. Therefore, 18 of the 24 pediatric and adult patients had ongoing complete responses at a median follow-up of 2.6 months after treatment.
The trials, a collaboration between The Children's Hospital of Philadelphia and the University of Pennsylvania, are overseen by Carl H. June, M.D., the Richard W. Vague Professor in Immunotherapy in the department of Pathology and Laboratory Medicine and director of Translational Research in Penn's Abramson Cancer Center.
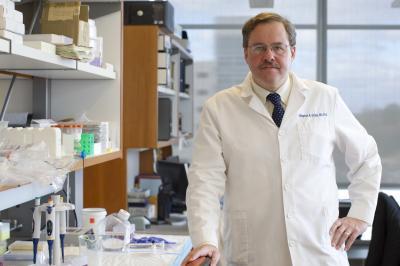
Stephan Grupp, M.D., Ph.D., is a pediatric oncologist and director of Translational Research at The Children's Hospital of Philadelphia Cancer Center.
(Photo Credit: The Children's Hospital of Philadelphia)
Grupp presented alongside Penn investigator Michael Kalos, Ph.D., during the press program. Kalos showed that measuring the number and activity of engineered T cells in patients with both ALL and chronic lymphocytic leukemia (CLL) who were treated with this investigational approach provided a useful gauge of treatment success.
A relatively new approach in cancer treatment, this type of immunotherapy relies on T cells, the workhorses of the body's immune system. Because B cells become cancerous in specific leukemias such as ALL, CTL019 cells function as cancer hunters, killing the leukemia cells that normally evade regular T cell surveillance. Researchers first extract a patient's own T cells and genetically modify them in Penn's cell and vaccine production facility to create CTL019 cells. Bioengineering techniques are used to reprogram each patient's T cells into chimeric antigen receptor cells—the CTL019 cells—custom-designed to bind to a protein called CD19 that exists only on the surface of B cells. Then, the cells are returned to the patient's body, where they proliferate and then eliminate B cells. Moreover, they persist in the circulation, helping to guard against the cancer's recurrence.
The current study reflects an ongoing collaboration between Grupp and the Penn Medicine scientists who originally developed this personalized cell therapy as a treatment for adult patients with CLL, another B-cell leukemia.
The CHOP/Penn research colleagues adapted the CLL treatment for use against a high-risk form of ALL. The most common childhood cancer and the most common childhood leukemia, ALL may also occur in adults, such as the five adult patients in the current trial.
"Although most adults with ALL respond to drug treatment, as many as half of them eventually relapse, putting the overall cure rate for the disease only around 40 percent," said David L. Porter, M.D., a professor of Medicine and director of Blood and Marrow Transplantation in Penn's Abramson Cancer Center, who leads the adult CLL and ALL trials along with Noelle Frey, M.D., an assistant professor of Medicine. "Once a patient relapses, treatments are often ineffective. Many of these patients are not even eligible for bone marrow transplants, so this approach stands to give them an option where they would otherwise have had none."
As the CTL019 cells potently attacked leukemia cells, they also stimulated an unwanted, toxic immune response called cytokine release syndrome. The care team successfully counteracted these side effects with two immunomodulating drugs. In addition, because the CTL019 therapy eliminates healthy B cells along with cancerous B cells, patients must receive infusions of immunoglobin to perform the immune function provided by normal B cells.
"The results from the ALL and CLL trials also demonstrate that these engineered hunter cells greatly expand in patients, producing very high complete response rates, and then persist in patients, potentially allowing for long-term disease control. We are looking forward to testing these cells in upcoming multicenter pediatric and adult trials," said Grupp.




Comments